The U.S. healthcare system is undergoing a fundamental shift from the traditional fee-for-service (FFS) model toward bundled payment models [1]. However, debate remains over which services are well-suited for bundled payments and which are not. In this blog, we explore this question by summarizing a systematic review published in Health Affairs, which examined the impact of bundled payments on healthcare spending, utilization, and quality [2]. The review analyzed 20 studies published between 2016 and 2019.
This blog is organized as follows:
- What is FFS and Bundled Payment Model?
- History of Bundled Payment
- Performance Measures of Bundled Payment Model
- Bundled Payment Impact on Healthcare Spending
- Bundled Payment Impact on Service Utilization
- Bundled Payment Impact on Quality of Care
- Unintended Consequences of Bundled Payment
- Which Procedures Are Best Suited for Bundled Payments?
- Conclusion
What is FFS and Bundled Payment Model?
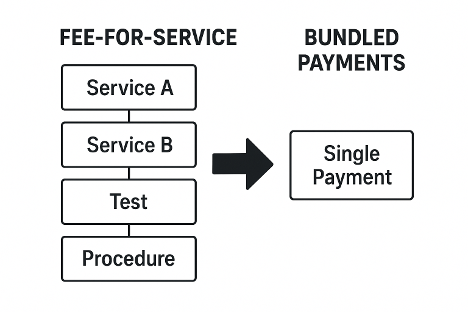
In the traditional FFS model, healthcare providers are paid separately for each service, test, or procedure they perform.
FFS: More procedures = more payments
In bundled payments model, there’s one fixed price that covers everything—like the facility fee, anesthesia, lab tests, and more. Many independent providers prefer this approach because it streamlines payments, reduces administrative burden, and incentivize quality outcomes [3, 4].
History of Bundled Payment
- Acute Care Episodes (ACE) – Launched in 2009, this program introduced bundled payments in acute care settings.
- Bundled Payments for Care Improvement (BPCI) – Launched in 2013; this program covered bundled payment for forty-eight episodes.
- Comprehensive Care for Joint Replacement (CJR) – Launched on 2016; this program applied bundled payments to hip or knee replacement surgeries.
Performance Measures of Bundled Payment Model
The effectiveness of bundles is measured in the following dimensions:
- Healthcare Cost Spending: measured using total episode spending.
- Utilization: measured using discharge destination, length of stay.
- Quality: measured using re-admissions, complications, mortality, ER visits.
- Unintended Consequences: measured using risk selection, case complexity, volume changes.
Unintended Consequences of Bundled Payment
Researchers also examined whether bundled payments might create unintended consequences. One concern was that hospitals could avoid treating high-risk or complex patients who might push costs above the target bundle. The review, however, found no consistent evidence of systematic risk avoidance, though some single-center studies suggested it could occur in certain situations. Another worry was that hospitals might increase procedure volumes simply to take advantage of bundled payment incentives, but the evidence showed no significant rise in surgical volume.
Bundled Payment Impact on Healthcare Spending
The clearest financial impact of bundled payments was observed in lower extremity joint replacement (LEJR) episodes, such as hip and knee replacements. These procedures are relatively standardized and predictable, making them ideal for bundled payment models.
- LEJR Savings: Multiple studies demonstrated meaningful cost reductions, with one multicenter study showing a $1,166 (3.9%) savings per episode under BPCI. Much of this came from reduced reliance on costly post-acute care services (like inpatient rehabilitation and skilled nursing facilities).
- Other Conditions: For procedures with more variability—like spinal fusions—results were mixed, with some studies even reporting increased costs due to the complexity of patient needs. Cardiac surgeries showed inconsistent results, with no clear evidence of sustained savings.
- Medical Conditions: Episodes for chronic or acute medical conditions (such as COPD, pneumonia, sepsis, or heart failure) generally showed no measurable savings. These conditions involve more unpredictable care pathways, making cost standardization much harder.
| Condition | Spending Impact |
|---|---|
| Hip/Knee Replacements (LEJR) | ↓ Significantly lower |
| Spine Fusion | Mixed/No savings |
| Cardiac Surgery | No consistent savings |
| Medical Conditions (COPD, Sepsis, etc.) | No savings |
Bundled Payment Impact on Service Utilization
Bundled payments also changed how care was delivered after hospitalization, not just how much it cost. Hospitals participating in these programs were less likely to discharge patients to post-acute care facilities such as skilled nursing or inpatient rehabilitation centers, and instead, more patients were sent home or managed with less intensive support. Across multiple studies, the average hospital stay decreased by 0.3–1.4 days, suggesting that care was being streamlined without adding risk to patients. Similarly, for those who were discharged to post-acute facilities, the average length of stay was modestly reduced, contributing further to overall cost savings.
Bundled Payment Impact on Quality of Care
One major concern with cost-cutting programs is whether quality of care suffers. Encouragingly, bundled payments showed neutral to positive results in most cases. Several studies found reductions in readmissions of up to 7 percent, particularly among lower extremity joint replacement patients, which is an important indicator of better care coordination. Other quality measures, including complication rates, mortality, and emergency department visits—showed no significant differences compared to fee-for-service, suggesting that hospitals were not compromising patient safety or outcomes in their efforts to save money. In short, quality largely remained stable, and in some cases, such as re-admissions, it even improved while overall costs declined.
Which Procedures Are Best Suited for Bundled Payments?
- Bundled payments work best for elective, standardized procedures (like hip/knee replacements).
- Medical conditions (e.g., COPD, sepsis) are harder to fit into bundles due to higher patient complexity.
- Risk stratification is critical – bundle payment should adjust payments for complex patients to avoid discouraging hospitals from treating them.
Conclusion
Bundled payments have demonstrated clear potential in reshaping healthcare delivery, particularly for standardized procedures like joint replacements where they consistently lower costs without compromising quality. However, their impact on more complex medical conditions remains limited, highlighting that a one-size-fits-all approach may not work. As the U.S. healthcare system accelerates its shift toward value-based care, bundled payments could serve as a cornerstone reform but only if they are applied selectively, with careful attention to patient complexity, risk adjustment, and thoughtful program design to ensure fairness and sustainability. At Care Cadet, we are building a bundled care network for independent providers, including imaging centers, ambulatory surgical centers, and more. If you are an independent provider interested in joining our network, please contact us at info@carecadet.com.
References
- [1] https://www.cms.gov/priorities/innovation/innovation-models/team-model (Accessed: Sept. 21, 2025)
- [2] Agarwal, R., Liao, J. M., Gupta, A., & Navathe, A. S. (2020). The Impact Of Bundled Payment On Health Care Spending, Utilization, And Quality: A Systematic Review: A systematic review of the impact on spending, utilization, and quality outcomes from three Centers for Medicare and Medicaid Services bundled payment programs. Health Affairs, 39(1), 50-57.
- [3] https://surgerycenterok.com/surgery-prices/ (Accessed: Sept. 21, 2025)
- [4] https://renovohealth.care/ (Accessed: Sept. 21, 2025)
